The Mechanism Behind How Circumcision Prevents HIV
Male circumcision has been shown to significantly reduce the risk of heterosexual men acquiring HIV, but what’s the underlying mechanism behind this protective effect? Understanding how circumcision works in preventing HIV transmission can help clarify why it is such an effective public health intervention. Below is an in-depth exploration of the biological and behavioral factors that explain this connection.
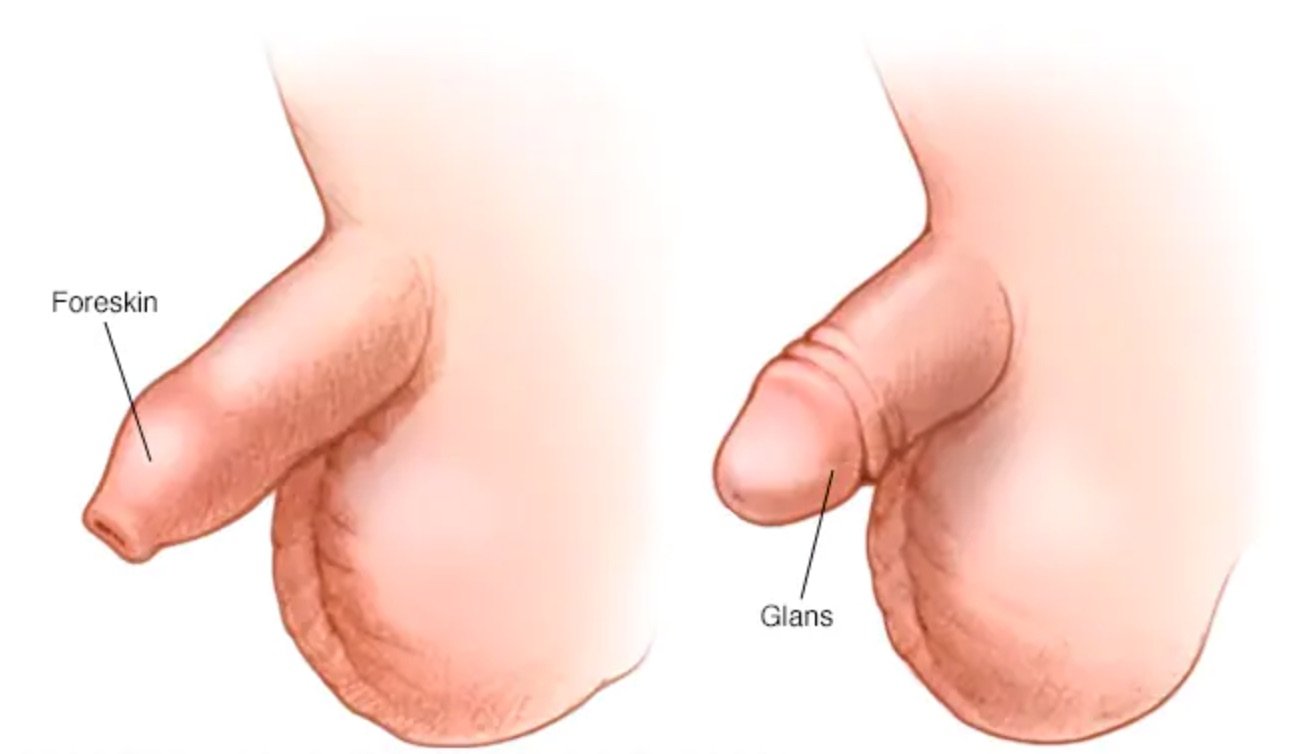
The Role of the Foreskin in HIV Transmission
The foreskin, a fold of skin covering the head of the penis (glans), plays a crucial role in how circumcision reduces the risk of HIV. Here are some of the key reasons why:
Presence of HIV-Targeted Cells: The foreskin contains a high concentration of specialized immune cells known as Langerhans cells, macrophages, and CD4+ T cells. These cells are primary targets for the HIV virus. When the foreskin is intact, these cells are exposed to the virus during sexual activity, increasing the risk of HIV entering the body and infecting these cells. By removing the foreskin through circumcision, the number of these target cells decreases, lowering the chances of infection.
Susceptibility to Microtears: During sexual intercourse, the foreskin is prone to developing microtears or abrasions, particularly in environments where sexual activity is frequent or condoms are not used. These small tears in the skin provide an entry point for HIV, allowing the virus to bypass the body's natural defense barriers. Circumcision removes this vulnerable tissue, decreasing the likelihood of microtears and thus reducing the opportunity for HIV to enter the bloodstream.
Decreased Moisture and Viral Survival: The foreskin creates a warm and moist environment, which is ideal for viral survival. This environment can increase the persistence of the HIV virus after exposure during sexual activity. When circumcision removes the foreskin, the penile surface becomes drier and more keratinized (hardened), reducing the likelihood that the virus can survive long enough to establish an infection.
Reduction of Co-infections: Circumcision has also been shown to lower the risk of other sexually transmitted infections (STIs), including syphilis, human papillomavirus (HPV), and herpes simplex virus type 2 (HSV-2). These STIs can increase the risk of HIV transmission by causing inflammation or ulcers on the genital tissue, which weaken the skin’s barrier and make it easier for HIV to enter the body. By reducing the risk of these co-infections, circumcision indirectly lowers the risk of HIV acquisition.
Scientific Evidence Supporting the Mechanism
The effectiveness of circumcision in preventing HIV transmission is backed by robust scientific evidence from randomized controlled trials and observational studies, especially in regions like sub-Saharan Africa, where the HIV epidemic has hit hardest. Here’s a breakdown of the key findings:
Langerhans Cells as Primary Targets: Langerhans cells play a pivotal role in the early stages of HIV infection. Research has shown that these cells capture the virus and transport it to CD4+ T cells, which HIV primarily infects. By removing the foreskin, the concentration of Langerhans cells is significantly reduced, making it more difficult for the virus to initiate infection.
Keratinization of the Glans: Following circumcision, the glans (the head of the penis) undergoes a process called keratinization, where the outer layer of the skin becomes thicker and more resilient. This thickening serves as a protective barrier, making it harder for the virus to penetrate the skin and reach susceptible immune cells.
Decreased Inflammation: Inflammatory conditions on the genital surface are associated with a higher risk of HIV infection. Circumcision has been found to reduce chronic inflammation caused by bacterial infections that thrive in the moist environment under the foreskin. Reduced inflammation leads to fewer immune cells at the genital surface, making HIV transmission less likely.
The Importance of Circumcision in the US as a HIV Prevention Strategy
During the HIV epidemic, high rates of circumcision in the United States were seen as beneficial in reducing the spread of HIV, particularly among heterosexual men. Research conducted in Africa and other regions demonstrated that circumcision reduced the risk of heterosexually acquired HIV infection in men by approximately 60%. This is because, as mentioned above, the foreskin contains cells that are particularly susceptible to HIV infection, and removing it reduces the surface area through which the virus can enter the body.
In the U.S., where circumcision rates have historically been high, especially among newborn males, this preventive factor contributed to a lower transmission rate in certain populations. Public health experts took note of these findings during the HIV crisis and encouraged circumcision as part of a broader HIV prevention strategy, particularly in regions with high rates of HIV transmission.
While circumcision alone is not enough to prevent HIV, in combination with other methods like condom use, antiretroviral treatments, and education, it became one of several tools to help reduce the spread of the virus. This global research helped reinforce the potential health benefits of circumcision in the U.S. context during the height of the epidemic.
The Importance of Circumcision in HIV Prevention Strategies
It’s important to emphasize that circumcision should not be viewed as a standalone solution to preventing HIV but rather as part of a comprehensive approach to sexual health. The following elements should complement circumcision for maximum protection:
Condom Use: Circumcision reduces the risk of HIV but does not eliminate it. Using condoms consistently remains essential for reducing transmission during sexual activity.
HIV Testing and Counseling: Regular HIV testing and counseling are vital for identifying and managing HIV status early, particularly for those in high-risk populations.
Antiretroviral Therapy (ART): ART helps individuals living with HIV reduce viral load and prevent onward transmission. It should be widely accessible alongside circumcision efforts.
Conclusion: A Scientific Approach to HIV Prevention
Circumcision reduces the biological pathways through which HIV can enter and establish infection in the male body, offering significant protection. However, it is most effective when combined with other preventive measures like condom use and regular HIV testing. Understanding these mechanisms highlights the importance of circumcision as part of a broader public health strategy for reducing the global impact of HIV, in the US and other parts of the World.
SafeCirc is dedicated to promoting long-term health benefits through early circumcision, ensuring that the procedure is done in a safe, sterile environment for infant boys. By choosing circumcision, parents can contribute to their child's lifelong protection against serious infections like HIV.